
Broad consent is increasingly recommended as an acceptable consent model for biobanking human samples and health data with a view to their future use in research. Empirical evidence on the practice of broad consent and its implementation in the hospital setting, however, is still very limited. We analyse and discuss results from a qualitative study of perceptions of a sample of patients and biobank recruiters regarding broad consent to participate in a hospital-based biobank for prospective research on genomic and health data. Our findings suggest that contextual and relational factors play an important role in the practice of broad consent, and illustrate that broad consent relies as much on intuition as on reasoning. Moreover, we show that seeking broad consent in the hospital affects patient-recruiter interaction and that “conditional” trust plays a significant role in broad-consent decision-making. In conclusion, we provide recommendations to improve patient autonomy in the context of hospital-based broad consent.



As long as relevant information is provided and ethical safeguards are guaranteed, broad consent is increasingly recommended as an acceptable consent model for biobanking human samples and health data with a view to their future use in research [1]. Research on broad consent has considered its ethical acceptability either on the basis of the normative values it conveys [2,3,4,5,6], or in comparison with other consent models for prospective research on human samples and data [7,8,9,10]. Studies on public perceptions have shown that there is little consensus about broad consent being the most appropriate model for prospective biobanking and data collection [11]. However, there is still a paucity of data on the actual practice of broad consent for prospective research on genomic and medical data. Indeed, few studies have explored the influence of external persons in the decision to participate in population genetic research databases [12] and understanding is limited regarding what factors, other than motivational, may influence the decision whether to participate in biobank research using broad consent. Hence, there is an urgent need for implementation research in this field.
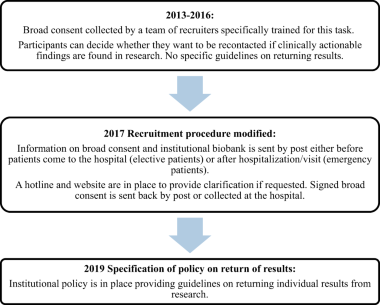
The Lausanne Institutional Biobank (BIL) was designed to improve research at the Lausanne University Hospital (Centre hospitalier universitaire vaudois, CHUV). Since 1 January 2013, in- and out-patients have been asked to donate a sample of blood (7.5 ml) and leftover tissue samples and give access to their health-related data. In accordance with the Swiss Federal Act on Research involving Human Beings [13], broad consent was chosen as the most suitable model [14]. According to this model, individuals consent to the broad, open-ended use of their samples and medical data in research, including genome analyses, as long as these projects have been approved by the local Institutional Review Board. In addition, BIL participants could accept or not to be re-contacted if clinically actionable findings are found in research. From 2013 to 2017, patients’ consent was collected by a team of recruiters at the CHUV (nurses, medical assistants and research personnel) specifically trained for this task. In 2017, the BIL recruitment procedure was significantly modified: patients are now sent information on the biobank by post before they come to the hospital and a hotline is in place to provide clarification and additional information if requested; signed consent forms are collected by healthcare professionals on patient’s arrival (see Box 1 on the development of broad consent in the CHUV).
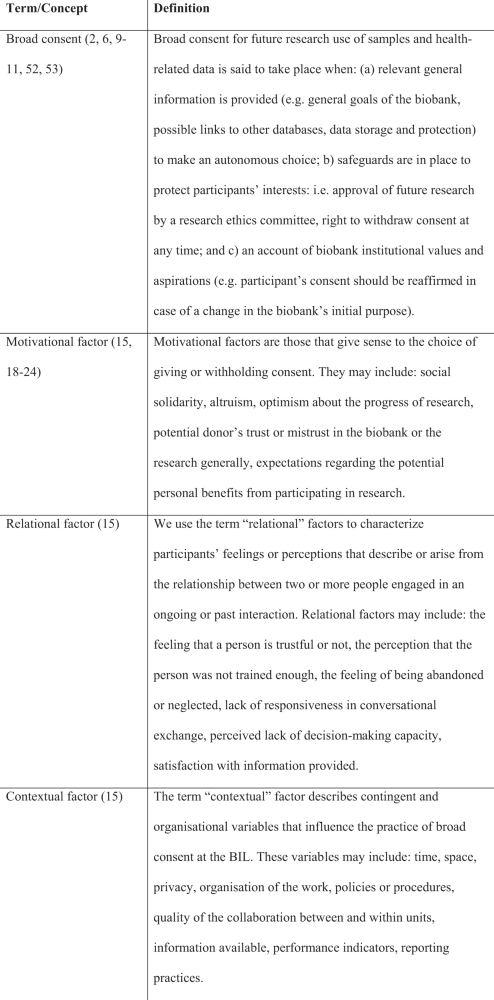
Our study on the 2013–2015 procedure for recruitment within the BIL, involving the team of recruiters, provided us with empirical evidence on the process of recruitment, motivation for participation and non-participation in a biobank and the practice of broad consent in a hospital setting. In this paper, we analyse and discuss qualitative data describing the meeting between patients and BIL recruiters. The aim is twofold: first, we identify motivational, relational and contextual factors ([15]; see also Box 2 for definitions) that may affect the decision-making process about broad consent; secondly, we examine aspects of the broad consent process that could be improved. With respect to existing literature on broad consent to research, the particularity of this study is to provide a first insight into the implementation of broad consent when practiced within a hospital setting. This is achieved through comparing the views of recruiters and patients whilst taking into account contextual factors that may affect recruiter–patient interaction and decision-making.
Purposive samples of patients and staff were drawn up, designed to obtain as diverse a population as possible according to identified key characteristics (patients: decision regarding participation, sex, age, hospital service, recruiter, and mode of recruitment—i.e. oral information during the hospital stay vs. an ambulatory consultation; recruiters: hospital service, seniority as a BIL recruiter). Exclusion criteria for patients were: refusal to participate, insufficient knowledge of French or health conditions that would limit capacity to participate in interviews or lack of sufficient decision-making capacity at the moment of the interview. Potential participants were first seen by a nurse practitioner in order to establish if they were interested in participating in an interview about their perceptions of broad consent for the BIL. If they agreed, potential participants were provided with an information and interview consent form and their contact details passed on to the researchers (FB and DK). Researchers called potential participants about 1 week after the first contact with the nurse practitioner in order to give a short oral explanation, answer questions, and set up an appointment. All the patients referred to the researchers by the nurse accepted to participate to the interviews.
Participants in the focus groups were recruited by e-mail. In order to increase participation, focus groups were organised during a normal working day with the help of BIL managers. Participation was voluntary and the identity of the recruiters participating in the focus group was not disclosed to BIL managers by the researchers. FB and GB supplied the written information and the consent form to focus group participants 1 week before the meeting. The first 10 min of each focus group were dedicated to questions and collecting the signed consent forms.
The study received approval from the local Institutional Review Board.
Interview and focus group guides were developed based on a preliminary literature review [16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35] and the material made available by the BIL managers. Themes addressed in interviews and focus groups are listed in Table 1. Interviews were conducted by two independent investigators (FB and DK) and scheduled according to the wishes of the patients. Focus groups brought together participants in a quiet conference room in the hospital building and were conducted by two people: a moderator (FB), leading conversations on the basis of the guide, and an observer (GB), noting participants’ non-verbal expressions.
Table 1 List of the themes addressed in interviews and focus groups.In order to provide participants with suitable time for reflection, they were orally informed about the study’s aims and procedures by a researcher when first contacted to check for eligibility to participate in the interview or the focus group. Additional oral and written information and a consent form were provided at the time of the interview or focus group. Interviews and focus groups were audio-recorded and transcribed verbatim. All personal data were removed from the transcripts in order to protect participants’ identity.
Thematic analysis was carried out by FB and DK in order to identify codes from the data [36]. Constant inter-judge comparisons and collective discussion on meaning and coding ensured that categories were consistent. To check coding reliability, the interview and focus-groups transcriptions were cross-checked. Encoding disagreements were resolved with reference to the raw data. On this basis, descriptive accounts were written and discussed by all the research team. Findings from interviews and focus groups were compared in order to check the consistency of the resulting categorisation and to increase methodological reliability [37].
We carried out 22 semi-structured interviews with patients who had agreed (n = 16) or refused (n = 6) to participate in the BIL and two focus groups with two different groups of biobank recruiters (n = 13). Patients’ characteristics are depicted in Table 2. The first focus group was composed of eight recruiters, the second focus group consisted of six recruiters. Given the small size of the groups, recruiters’ characteristics are not disclosed in this paper in order to protect their identity and the confidentiality of their remarks.
Table 2 Interviewee characteristics.Our findings elucidate the perceptions of a sample of patients and recruiters about the practice of broad consent to participate in a hospital-based biobank for prospective research on genomic and health data. The results of the analysis of the interviews with patients and of the focus groups with recruiters provided us with two different sets of data, each representing two sets of perceptions of the broad consent process implemented in the BIL biobank. Comparison of these data provided a fairly comprehensive picture of the motivational, relational, and contextual factors affecting the decision-making process about broad consent (see Box 2 for definitions). Below, we use exemplary quotations from the interviews and focus groups to illustrate our arguments.
Results from the interviews and focus groups show that seeking broad consent in a hospital setting has a direct influence on recruiters’ behaviour and the organisation of their work, patients’ understanding of broad consent and patient–recruiter interaction.
Biobank recruiters talked about their concerns around patient recruitment in a hospital setting. The first concern is linked to assessing the patient’s capacity to give consent. Some patients, for example, may be disoriented due to a psychological or health condition or their advanced age. The recruiters reported that caregivers are not always cooperative in reporting the patient’s actual capacity. The second concern relates to the timing of consent and the length of the meeting. Most patients are enthusiastic about the opportunity to talk with the recruiters as a way to escape from the tediousness of their hospital stay. However, since the recruiters visit the patients in their hospital rooms, caregivers performing routine daily care may interrupt the meeting. Also, the patients normally share their rooms with other people, which may compromise the patient’s propensity to discuss personal topics.
These difficulties may result in a stressful working environment for biobank recruiters, and more importantly, may affect patients’ understanding. Results from patient interviews show that some patients who agreed to participate in the BIL did not recall that broad consent also allows the hospital to collect data in forthcoming hospital stays without updating their consent. For other people, it is not clear that if they sign and accept the broad consent, researchers will be able to access their personal medical data. The possibility of a return of clinically actionable individual research results and the implications for the patient and his/her family also do not seem to be fully understood.
Results from interviews show that both patients who agreed and refused have positive attitudes towards biomedical research and, by extension, towards biobanking. Willingness to participate in the biobank depends on patients’ trust in the bona fide nature of the hospital institution.
This trust is sometimes inferred from recruiters’ behaviour. The quotations below show a positive and a negative example. Interviewee 13 refused to contribute to the BIL. He justifies part of his decision in terms of his perception of the recruiter:
“So, [the recruiter] was not a scientist. She was very kind, very kind, and sensitive but (chuckles) she was not…
Yes… (…) I felt that I had someone in front of me that did not have the competence to answer my questions.”
Interviewee 16, on the other hand, was satisfied with the meeting:
“The meeting was good. I felt the recruiter was open to all the questions I could have and… no, no, we took the necessary time to discuss…”
The recruiters also perceive that trust depends on their behaviour. Most of them saw themselves as biobank “ambassadors” and hospital representatives. Accordingly, recruiters make a special effort to behave in what they perceive as a professional and honest manner, so that they are worthy of the patient’s trust. This includes compensating for the lack of empathy and time sometimes experienced in the hospital setting…:
“Some patients will tell us things that they don’t want to tell the nurse or the doctor. Things that feel wrong, that they tried to tell the nurse, and to which she replied dryly since she has lot of stuff on her mind.”
…and for the inherent uncertainties of broad consent, as any possible future research use of samples and medical data is not known at the time of consent:
“We are completely honest since we don’t know exactly what project will be conducted. We cannot give them details about future research projects.”
As a consequence, broad consent could attest to a relationship of trust established by the biobank recruiters, rather than purely to understanding and agreement of the information provided in the consent process.
Moreover, results from our interviews with patients mostly show that participation in biobanking is motivated by altruistic reasons. People are likely to participate in order to support research and contribute to the progress of medicine in the common interest. They are generally aware that the results of future research may not benefit them personally. Several patients consider the decision to participate in biobanking as a way of feeling useful and hence as personally rewarding:
“I feel worthy… it is satisfying to tell myself that this can be useful to someone or to medical research in general.”
The recruiters were aware of this feeling. One recruiter, for example, suggested that some patients may perceive their participation in the biobank as edifying since they were asked to actively contribute to research and symbolically escape their role as passive recipients of care:
“The nurse, she has something to do to patients. Whereas we, we have something to ask of patients.”
It is notable, however, that patients who give their broad consent agree that donation to biobank-based research would only make sense as a collective endeavour. They are aware that the individual decision to participate in biobank research is worthwhile only if many other patients give their consent.
As individuals who have experienced disease and benefited from healthcare, several patients also explain their participation as a way of giving back the healthcare benefits they have received. In this sense, some patients insist on the importance of returning benefits to the hospital that took care of them, while others refer to a more general motivation to return the benefits they had out of medical research. These patients perceive themselves as “donors” rather than “participants”, and compare biobank participation to blood and organ donation:
“(Organ donation), I could do that, it’s something I could see myself doing—especially knowing that I could save someone, help someone, (…), but yes, yes, for me it’s part of the same impulse, the same, the same intention.”
Patients had a mixed perception of the likelihood of being informed of individual results, some believing that they would be informed of these results, while others did not expect to receive more information from the biobank. When asked about their preferences, most patients indicated that they would like to be informed if research revealed information of significance to their health. In their opinion, this information would concern either the discovery of a new treatment from which they could benefit or indications of preventive behaviour to adopt with regard to the risk of developing a particular disease. A minority of patients were more cautious and indicated that awareness of being at risk of developing a particular disease may be a cause for concern and anxiety. Our study, however, does not provide conclusive evidence on the role played by the perspective of a return of individual research results as a motivational factor for patients. When asked about this topic, recruiters once again highlighted the disinterested nature of patient’s willingness to participate in the biobank by pointing out that, in their opinion, the return of results did not seem to be determinant in patients’ decisions. However, it is difficult to be categorical about this conclusion because recruiters admitted that they themselves tended to minimise the possibility of a return of results by stressing, on the one hand, that biobank research was not yet defined and, on the other, that a return could take place in the very distant future. It is worth noting that at this point of the biobank development there were no policies or guidelines ruling the return of results to participants (see Box 1 on the development of broad consent in the CHUV).
Both patients who accepted and those who refused to give broad consent expressed several concerns about the use of samples and data in biobank-based research. Some patients are uncomfortable with the uncertainties associated with broad consent, mostly related to the vagueness of future research. Most patients feel it is difficult to anticipate the concrete use of their samples and data, or are confused when asked about research that may be conducted within the biobank. Several patients who refused to give broad consent expressed a preference for a specific consent, which they associate with more transparency about the contents and directions of biobank research.
Moreover, patients considering participation in the biobank as a risk worry that their samples and data may be used against their interests. Specifically, patients are concerned about data being made available to insurance companies, employers and medical institutions. Also, some feel that research on their biological sample could open the door to stigmatisation or discrimination, such as the denial of care:
“Let’s admit it, there are a lot of data in the biobank at the moment with my name on them. Now, here I am in the hospital and my heart is getting worse and worse, and they ask themselves the question: ‘Are we going to operate, or do a transplant, or God knows what?’, and these doctors are going to get data from the biobank, data about life expectancy, for example. About my life expectancy, and then they’ll say: ‘OK, but look, his life expectancy is only six years so it’s not worth doing anything.’”
Patients were sometimes worried that future biobank research on their samples or data might be contrary to their own ethical values and explicitly expressed concerns about vexed issues such as human cloning or eugenics. Sometimes, patients expressed their reluctance to support research that resulted in profits for pharmaceutical companies. They associate pharmaceutical companies with an inequitable distribution of profits, conflicting interests in research and the potential misuse of data and samples, and claim that the results of biobank research should remain in the public domain:
“(…) I mean there was no, err … guarantee that the pharmaceutical industry couldn’t use the data for its own ends, so the reason I refused was because I think that if someone wants to have these data, we’re the ones who should be holding them, science is what should be holding them, whether that’s the CHUV, or another institution, but in any case, not a pharmaceutical company, which would use them for its own benefit. We know that sometimes, health and the pharmaceutical industry don’t share the same goals.”
Results from focus groups with the biobank recruiters and members of the operational management team at the BIL are consistent with these findings. Narratives confirm that patients regularly ask questions about future research and the use of samples and data by private companies or other institutions. Members of the BIL management team insisted that patients’ concerns are adequately addressed through oversight of the use of future research provided by the scientific committee of the BIL and by the cantonal Ethical Review Board. However, even though potential participants are informed of these safeguards, patients who refused to participate in the BIL remain ambivalent and express concerns about potential conflicts of interest that may arise in ethical evaluation of the use of future research, in particular when public-private partnerships are in place.
We acknowledge that the results presented above have certain limitations. Even though we selected interviewees in such a way as to take into account the variability in patients recruited to participate in the BIL, it is possible some aspects of variation escaped us owing to the small number of interviews conducted. The focus groups, on the other hand, involved the majority of the recruiters employed at the BIL at that time. Nevertheless, discussion guides were designed to focus on specific aspects of their activity and their interpretation of their meetings with patients at which we were not present. For these reasons, any generalisation of the results presented in this paper must be cautious.
The comparison of the results of the interviews with participants in the BIL and of focus groups with BIL recruiters allowed us to highlight the weight of factors other than motivational issues in broad consent to genomic medicine. Our findings show that contextual and relational factors play an important role in the practice of broad consent. Specifically, when broad consent is sought in a hospital setting, patient–recruiter interaction can be significantly affected. Indeed, contextual factors, such as the limited time available for the encounter between patient and recruiter and frequent interruptions for daily care routines, have an impact both on recruiters’ attitudes and patients’ understanding. Numerous studies have highlighted that the practice of obtaining informed consent to elective surgery or research is subject to many legal and organisational constraints, to the point that several scholars have questioned the current ethical validity of informed consent. However, to the best of our knowledge, this is the first study that investigates the influence of organisational and other contingencies on the practice of broad consent.
With regard to relational factors, our results suggest that, in order to cope with the challenges of in-hospital recruitment and with the uncertainties associated with broad consent, biobank recruiters endeavour to establish an empathetic relationship with the patients and behave in a trustworthy manner. In addition, the interviews highlight that perception of the recruiter plays a role in the patient’s decision. Overall, these results suggest that rational and informational accounts of broad consent [6, 9], according to which people make sound and autonomous decisions when provided with factual information, are insufficient to explain participation in biobanks. At the BIL, participation in a biobank and granting broad consent seem to rely substantially on the perception of the recruiter and/or the institution. Therefore, the decision to participate or not in a biobank may depend as much on participants’ past experiences and beliefs, referred to by Hermann, Trachsel, and Biller-Andorno as “intuition”, as on information and participants’ assessment of risks and benefits [38]. In other words, their reasoning is implicit rather than explicit. Accordingly, our results are consistent with evidence from recent empirical studies showing that research participants’ preferences about the use of their samples and data are deeply influenced by relational considerations [39].
Findings from our study are also in line with the existing literature on the role of trust in people’s willingness to participate in biobanking [19, 40, 41]. Moreover, our results are consistent with evidence from a pan-European study of people’s willingness to participate in biobanking, showing that biobank participants’ trust is not absolute, but rather conditional on the trustworthiness of research institutions [32]. In the same line of argument, our findings indicate that the decision to give broad consent to hospital-based biobanking results from the balance between trust in healthcare professionals and the hospital institution and the potential risks involved in biobank participation.
Our results are also consistent with recent empirical work on biobank participants’ narratives about donation [42], showing that participants consider their contribution to biobanking as an unconditional gift, made with no expectation of a return of personal benefits, and as a “collective gift”, that is, a gift for our collective social good. On the basis of our results, we further argue that this attitude about biobank participation should be considered rather as an effect of the broad consent process in the hospital setting than as an argument to conceptualise broad consent as based on a purely altruistic participation in research. Such a conclusion would be reductive since we also found that, in the hospital setting, patients understand biobank participation both as a “reciprocal” gift, i.e. a way to return healthcare benefits from biomedical research, and as a “conditional” gift, i.e. a gift that is worthwhile, as long as the hospital institution supporting biobank research is trustworthy. We claim that such a “conditional” trust is fragile and, as illustrated by controversy sparked among research participants in a prominent direct-to-consumer genetic testing company [43], could be put at risk if the institutions supporting research are not transparent with regard to the use of data and samples in research.
While patients interviewed in our study expressed a great sense of trust in the hospital as a publicly funded research institution, they also showed no trust in private companies, in particular the pharmaceutical industry. The same results were reported in several earlier studies with patients and the public [44]. We support the idea that these concerns may be counterbalanced by more transparency about possible uses of research and exploitation of biobank research results [10, 39, 45, 46]. This approach should also involve the implementation, alongside a broad-consent model, of a biobank governance framework including patients’ and community representatives [47]. Citizens’ inclusion in the governance of the biobank may fill the gap between the public’s concerns and the safeguards proposed at this point and accordingly, improve people’s trust and participation.
Although care should be taken in generalising from these results, lessons can be learned from the BIL’s handling of broad consent in a hospital setting. These lessons are particularly relevant for the Swiss context, where a Federal template for broad consent to research on biological samples and medical data has recently been established. Footnote 1 Broad consent to the BIL specifically refers to research on genomic data in addition to health-related data in general. The federal template has a broader remit, and as such, our results have general relevance for future implementation of broad consent in Swiss hospitals, as they show the importance of motivational, relational and contextual factors for the patient’s decision-making process.
Several challenges may be associated with the implementation of broad consent in the hospital setting, such as: integration of recruitment within daily healthcare activities, limited time available for patient–recruiter interaction, potentially stressful conditions for recruiters (e.g. risk of being interrupted), and the possible lack of cooperation from healthcare personnel. Our results demonstrate that these difficulties have an impact on the interaction between the patient and the recruiter and should be carefully considered and addressed when seeking broad consent in a hospital context.
Our study shows that in order to conduct the interview within the expected timeframe and to cope with the complexity of the information and uncertainties associated with broad consent, recruiters endeavour to establish an empathetic relationship with patients and to present themselves as trustworthy representatives of the hospital. As a consequence, who conveys the information and how the information is conveyed has as much influence on the patient’s decision-making as the content of the information itself. We conclude that broad consent in hospital settings may rely more on intuition than on reasoning [38]. In order to respect patient autonomy, this should be taken into account when developing a broad-consent process, especially in the hospital setting.
Our results corroborate existing evidence that trust in healthcare institutions and healthcare providers is crucial to understanding patients’ willingness to consent to research on data and samples. With regard to broad consent in particular, our study shows that patients’ decision-making consists in weighing this trust against concerns about the potential risks associated with research (e.g. privacy risks). Moreover, our results indicate that, in the hospital setting, patients understand biobank participation as “reciprocal” and as a “conditional” gift that depends on the trustworthiness of the hospital institution. Potential concerns about uncertainties associated with broad consent should be addressed through more transparency about the possible uses of research [24]. Our results suggest that the high-participation rates observed for the BIL biobank cannot simply be understood in terms of public trust in research [48, 49]. We believe that, ultimately, the public’s and participants’ engagement in biobank governance is the way to achieve transparency, maintain trust, and ensure the success and longevity of biobanks [50, 51].
For more information, see the website of the Swiss Academy of Medical Sciences (https://www.samw.ch/fr/Ethique/Ethique-de-la-recherche/Modele-CG.html, last retrieved on April 7th, 2019) and of Unimedsuisse, the Swiss Association of University Medicine (https://www.unimedsuisse.ch/fr/projets/consentment-general, last retrieved on April 7th, 2019).
This study was funded by a grant of the Research Commission of the Département universitaire de médecine et santé communautaires (DUMSC, CHUV) and carried out by the Institute of Humanities in Medicine (UNIL-CHUV), in collaboration with the Institute of Social and Preventive Medicine (UNIL-CHUVl) and The ColLaboratory (UNIL). The authors warmly thank the management team and all the collaborators of the Lausanne Institutional Biobank who made our study possible and provided essential insights into the issues discussed in this article. They also thank Murielle Bochud and Lazare Benaroyo, co-applicants of the study, for their support and collaboration in the design of the research, and Alain Kaufmann for his contribution in designing the study, preparing the fieldwork and analysing results.